SomnusNooze
Researchers have provided more evidence that narcolepsy without cataplexy (Nw/oC ) and idiopathic hypersomnia (IH) without long sleep time (LST) look more alike on testing than do narcolepsy with cataplexy (NwC) and Nw/oC.
This research was completed before the publication of the International Classification of Sleep Disorders (ICSD-3) in 2014, and therefore the researchers based their classifications on ICSD-2 criteria.
Background
Over the past few years as researchers have studied the spectrum of hypersomnolence disorders, they not only have separated narcolepsy into two types (now called type 1 [T1N] and type 2 [T2N] in ICSD-3), but also have identified factors that differentiate the central disorders of hypersomnolence. These factors, also called markers, include hypocretin levels, the results of HLA typing, and measures of sleep obtained via the Multiple Sleep Latency Test (MSLT) and one or more of the following: actigraphy, polysomnography, and sleep diaries.
Several recent research studies have determined that these “narcolepsy markers” are less likely to occur in people with T2N than in people with T1N and that people with T2N have markers that are more similar to those of folks with IH than those with T1N. For example, fewer than 40% of patients with TN2 are HLA positive (that is, they have at least one allele for DRB1*1501/DQB1*0602). This is particularly interesting given the fact that 24% of the general population is HLA DRB1*1501/DQB1*0602 positive. (This percentage varies depending on race.) In addition, only 30% to 40% of people with T2N have sleep paralysis or hypnagogic or hypnopompic hallucinations.
Although the consensus of an expert panel published in 2013 was that people with narcolepsy experience disturbed night-time sleep (DNS), and subsequent publications have supported this idea, no studies conducted until now nor the consensus panel itself have examined DNS and differentiated between patients with and without cataplexy or between those without cataplexy who are or are not HLA positive.
Who were the research participants and what did they do?
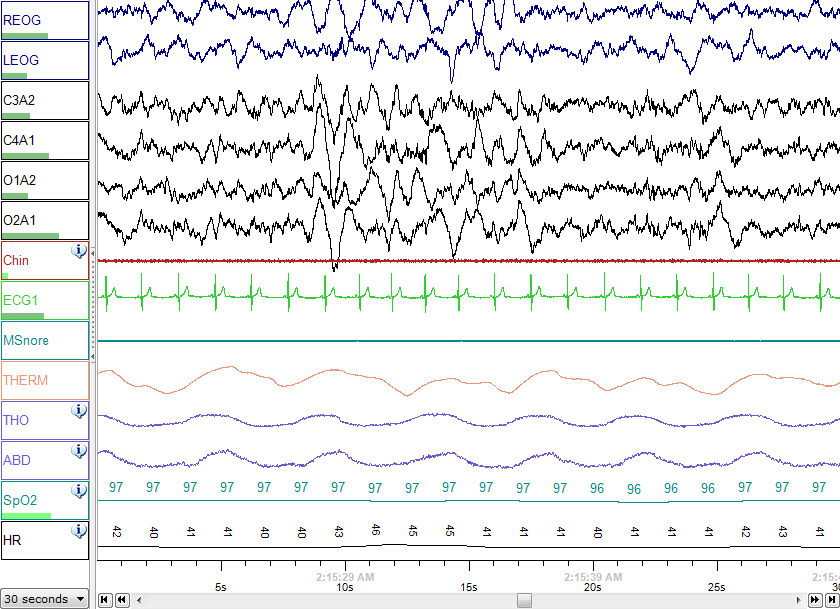
All of the participants were Japanese, visited the Japan Somnology Center at some time between 2003 and 2008, and had hypersomnia that had not been previously treated. They were all asked to obtain at least 6 hours of sleep per night and to maintain a regular sleep-wake cycle for two weeks before being studied in the sleep laboratory. They underwent in-laboratory, overnight polysomnography (including 4 channels of electroencephalography [EEG]), and an MSLT. All participants also had HLA typing, completed the Epworth Sleepiness Scale, and reported whether or not they had hypnagogic hallucinations or sleep paralysis.
Who were the researchers and what did they do?
Dr. Taeko Sasai-Sakuma and Dr. Yuichi Inoue at Tokyo Medical University and the Japan Somnology Center interpreted the results of the polysomnograms and MSLTs and specifically scrutinized the EEG data obtained during sleep and as the participants fell asleep (that is, waking EEG data).
What were the results of the study?
The following people took part in the study
| Sleep disorder | Number |
| NWC | 28 |
| N w/o C and HLS+ | 16 |
| N w/o C and HLA- | 22 |
| IH w/o LST | 22 |
Those people who had NwC and Nw/oC HLA+ were much more likely to have hypnogogic hallucinations and sleep paralysis, as compared with people who had Nw/oC HLA-. In addition, on the MSLT, compared with all other groups, the IH group took longer to fall asleep, as did the Nw/oC HLA- group, when compared with the other two narcolepsy groups.
Analysis showed no differences in any polysomnographic parameters between the group with Nw/oC HLA- group and the IH group; however differences did exist between the combined NwC and Nw/oC HLA+ groups and the combined Nw/oC HLA- and IH groups with regard to wake time after sleep onset (more), time to REM sleep (shorter), arousal index (higher), sleep efficiency (lower), percentage of stage 2 sleep (lower), and likelihood of having sleep-onset REM periods (higher). Differences were also found between these two groups in terms of EEG measures during wake and REM sleep. No differences in EEG measures were found among any of the four groups during slow-wave sleep.
What were the researchers conclusions?
According to the authors, “The present results support the idea that the higher prevalence of REM-related symptoms in these two categories [NwC and Nw/oC HLA+] is attributable to instability of sleep–wake regulation and increased REM sleep propensity caused by hypocretin secretion deficiency.” They go on to further note that, “either the presence of cataplexy or HLA positivity, or both, is associated with DNS, EEG slowing during wakefulness, and intrusion of fast EEG activity during REM sleep in narcolepsy.” These characteristic polysomnographic findings seemed to be lacking in the Nw/oC HLA- and IH groups.
Source
Sasai-Sakuma T, Inoue Y. Differences in electroencephalographic findings among categories of narcolepsy-spectrum disorders. Sleep Med 2015 doi: 10.1016/j.sleep.2015.01.022. [Epub ahead of print].
