Narcolepsy type 1
with cataplexy

with cataplexy
 Narcolepsy type 1 (NT1) is a long-lasting (chronic) hypersomnia sleep disorder of the brain (neurologic disorder).
Narcolepsy type 1 (NT1) is a long-lasting (chronic) hypersomnia sleep disorder of the brain (neurologic disorder).
NT1:
NT1 is caused by problems with orexin, a chemical messenger for nerve cells (neurotransmitters).
Orexin:
Most likely, an autoimmune process (where your immune system makes your body attack itself) leads to low orexin levels and causes problems with these body systems.
Jump to page sections
Common symptoms include:
You don’t need to have all of these symptoms to be diagnosed with NT1, but you’ll have at least some of them.
To learn more about coping with some of these symptoms, visit Project Sleep’s web pages:
Episodes of cataplexy can be very different in how long they last and how intense they are. They may include:
You won’t lose consciousness, but it may look to others like you passed out or fainted. These episodes are often triggered by strong emotions such as laughter. If you think you may have cataplexy, take notes about your episodes (and video if possible) to discuss with your doctor.
Watch this short BBC video “What is it like to have a cataplexy attack”:
Symptoms most often start in a person’s mid-to-late teens. However, they can start at any age. They may start suddenly or develop over time.
Symptoms may:
If you have NT1, you may have times when you can function (do daily activities such as work or school) well or well enough, and other times when you don’t function well at all. Even if you function well at times, your symptoms should be taken seriously.
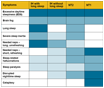 Visit our web page: “Compare symptoms of idiopathic hypersomnia and narcolepsy types 1 and 2.”
Visit our web page: “Compare symptoms of idiopathic hypersomnia and narcolepsy types 1 and 2.”
Researchers estimate that narcolepsy in general (including both NT1 and NT2) happens in 1 in 2,000 people. It’s harder to know how many people have NT1, but researchers estimate 1 in every 5,000 people to 1 in every 3,333 people have it.
NT1 can greatly affect daily life:
These effects are especially true for people who aren’t taking medicines that work well. But even with medicines, people who have NT1 may struggle with these activities.
While almost everyone with NT1 has EDS and cataplexy, not everyone has the other symptoms, and they can affect each person differently. Watch these videos to learn more:

![]() You may need to prepare during the weeks leading up to your sleep studies, and your doctor may recommend that you change or stop taking specific medicines. Ask for time off from school or work if your symptoms are likely to keep you from being able to function well while you prepare. This may happen if you need to:
You may need to prepare during the weeks leading up to your sleep studies, and your doctor may recommend that you change or stop taking specific medicines. Ask for time off from school or work if your symptoms are likely to keep you from being able to function well while you prepare. This may happen if you need to:
To learn more, visit our web pages:
The MSLT results doctors use to diagnose NT1 and NT2 are the same, so the results don’t help show which sleep disorder you have. Your symptoms, especially cataplexy, can help doctors tell the difference. If you don’t clearly have cataplexy, you may need to follow these steps to tell the difference between NT1 and NT2:
 If you’re a person of African descent, you may be more likely to have narcolepsy without cataplexy and with low orexin levels. This is the form of NT1 needing these extra tests for correct diagnosis. Read our article “Differences in Hypersomnia Disorder Symptoms Among African Americans.”
If you’re a person of African descent, you may be more likely to have narcolepsy without cataplexy and with low orexin levels. This is the form of NT1 needing these extra tests for correct diagnosis. Read our article “Differences in Hypersomnia Disorder Symptoms Among African Americans.”
Once your doctor diagnoses you with NT1, you usually don’t need to repeat sleep studies.
Visit our web pages:
Visit our web page for doctors: “Diagnosis, classification, symptoms, and causes of hypersomnias.”
Published Jan. 19, 2024 |
Revised Jun. 24, 2024
Approved by our medical advisory board