Narcolepsy type 2
without cataplexy
without cataplexy
 Narcolepsy type 2 (NT2) is a long-lasting (chronic) hypersomnia sleep disorder of the brain (neurologic disorder).
Narcolepsy type 2 (NT2) is a long-lasting (chronic) hypersomnia sleep disorder of the brain (neurologic disorder).
NT2:
NT2 is similar to idiopathic hypersomnia (IH) in some ways and to narcolepsy type 1 (NT1) in other ways. Researchers don’t yet know the cause of NT2, but it isn’t caused by the same problem as NT1.
Jump to page sections
The main symptom of NT2 is EDS that lasts for at least 3 months. Sleep patterns may also change, and if you have NT2, you may need 1 or more naps a day.
Common symptoms include:
You don’t need to have all of these symptoms to be diagnosed with NT2, but you’ll have at least some of them.
To learn more about coping with sleep-related hallucinations and paralysis, visit Project Sleep’s web page.
Symptoms most often start in a person’s mid-to-late teens. However, they can start at any age. They may start suddenly or develop over time.
Symptoms may:
If you have NT2, you may have times when you can function (do daily activities such as work or school) well or well enough, and other times when you don’t function well at all. Even if you function well at times, your symptoms should be taken seriously.
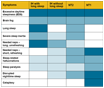 Visit our web page: “Compare symptoms of idiopathic hypersomnia and narcolepsy types 1 and 2.”
Visit our web page: “Compare symptoms of idiopathic hypersomnia and narcolepsy types 1 and 2.”
Researchers estimate that narcolepsy in general (including both NT1 and NT2) happens in 1 in 2,000 people. It’s harder to know how many people have NT2. Researchers have estimated 1 in every 5,000 people to 1 in every 3,000 people have it. Recent U.S. insurance claims data suggest it happens in 1 in every 1,500 people. However, estimates in Europe have been far lower.
NT2 can greatly affect daily life:
These effects are especially true for people who aren’t taking medicines that work well. But even with medicines, people who have NT2 may struggle with these activities.
Belle has narcolepsy, and the hardest things for her are falling asleep uncontrollably throughout the day and having frightening sleep-related hallucinations.
2020 October – Michelle Emrich, MD – “A Doctor’s Once Agile Brain Broken by IH” – Video courtesy of Michelle Emrich
Belle has narcolepsy, and the hardest things for her are falling asleep uncontrollably throughout the day and having frightening sleep-related hallucinations.
Find more personal journey stories on:

![]() You may need to prepare during the weeks leading up to your sleep studies, and your doctor may recommend that you change or stop taking specific medicines. Ask for time off from school or work if your symptoms are likely to keep you from being able to function well while you prepare. This may happen if you need to:
You may need to prepare during the weeks leading up to your sleep studies, and your doctor may recommend that you change or stop taking specific medicines. Ask for time off from school or work if your symptoms are likely to keep you from being able to function well while you prepare. This may happen if you need to:
To learn more, visit our web pages:
The MSLT results doctors use to diagnose NT1 and NT2 are the same, so the results don’t help show which sleep disorder you have. Your symptoms, especially cataplexy, can help doctors tell the difference. If your diagnosis still isn’t clear, you may need to follow these steps to tell the difference between NT1 and NT2:
 If you’re a person of African descent, you may be more likely to have narcolepsy without cataplexy and with low orexin levels. This is the form of NT1 needing these extra tests for correct diagnosis. Read our article “Differences in Hypersomnia Disorder Symptoms Among African Americans.”
If you’re a person of African descent, you may be more likely to have narcolepsy without cataplexy and with low orexin levels. This is the form of NT1 needing these extra tests for correct diagnosis. Read our article “Differences in Hypersomnia Disorder Symptoms Among African Americans.”
Visit our web pages:
Visit our web page for doctors: “Diagnosis, classification, symptoms, and causes of hypersomnias.”
Published Jan. 19, 2024 |
Revised Jun. 24, 2024
Approved by our medical advisory board
2020 October – Michelle Emrich, MD – “A Doctor’s Once Agile Brain Broken by IH” – Video courtesy of Michelle Emrich
Michelle Emrich is an internal medicine physician whose beloved career was cut short when she was 32 years old by the onset of severe, treatment-refractory idiopathic hypersomnia. In this video, she describes how IH broke her formerly agile brain, leading to unrelenting and painfully intense sleepiness, severe brain fog with associated cognitive dysfunction, and the need for multiple daily obligatory daytime sleep sessions. Michelle describes the huge impact of IH on every aspect of her life and the great importance of therapy and supportive healthcare providers. She hopes that sharing her story will help foster better understanding of this invisible disease.