SomnusNooze e-newsletter
News, stories and updates from the world of sleep
News, stories and updates from the world of sleep

On March 17, 2023, the Hypersomnia Foundation launches the premiere episode of LIVING WITH... a monthly YouTube series that expands awareness of idiopathic hypersomnia, healthy sleep habits, emerging research in sleep medicine, and more. Hosted by... read >

Mark Your Calendar and Save the Dates! The Hypersomnia Foundation is planning multiple opportunities for all of us to get together in 2023! Plan on connecting with others in the sleep disorder community with these HF events: UNIGHT - Enjoy a virtual... read >
November 29th is Giving Tuesday and we have much to be thankful for. We continue to listen to the community on our journey to improve as an organization for today and into the future. In June 2022, we hosted a successful #BeyondSleepy Conference for... read >

Are you a healthcare provider who is involved in research studies or the operation of sleep study centers? Or are you a researcher or a manager/team member of a sleep or research study site? If so, check out our new series of Guides for Professionals... read >

Happy 2022! If you’ve missed any of the latest news we’ve shared through our social media this month, don’t worry! Get up to date with this edition of “In Case You Missed It!” CONGRATULATIONS!: David Burley appointed as new Chair of HF's... read >
On this Giving Tuesday, as we reflect upon a year that has been challenging for all, we have much to be thankful for. We did not let the pandemic slow down or stop our progress. Instead, we continue to listen to the community on our journey to improve as... read >
Sleep hygiene—everybody, including both patients and healthcare providers, has heard that if these rules are followed, sleep will be improved. Right? What exactly are the official rules, and what’s not included? Should people who have IH or a related... read >
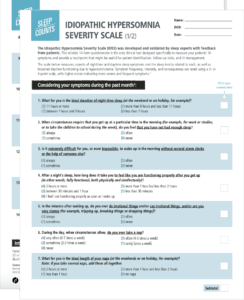
Take or administer this questionnaire now! The Idiopathic Hypersomnia Severity Scale (IHSS) is designed to help healthcare providers, researchers, and people who have IH monitor the severity of the spectrum of IH symptoms over time, including their... read >
Do you have idiopathic hypersomnia or a related sleep disorder, or do you treat patients with hypersomnias? If so, then check out our newly updated Treatment web page. Our Medical Advisory Board has just completed a full review and update, including... read >

Do you have idiopathic hypersomnia (IH) or a related sleep disorder or do you treat patients with hypersomnias? If so, then it’s very important to prepare in advance for anesthesia, hospitalization, and emergencies. People who have IH may face a unique... read >