SomnusNooze e-newsletter
News, stories and updates from the world of sleep
News, stories and updates from the world of sleep
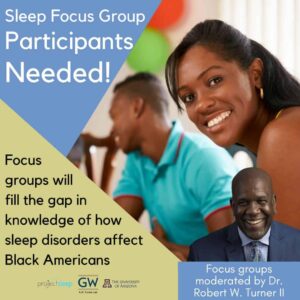
If you’ve missed any of the latest news we’ve shared through our social media, don’t worry! Get up to date with this edition of “In Case You Missed It!” Project Sleep is seeking Black American adults with sleep disorders for an upcoming... read >

The Hypersomnia Foundation held our first #BeyondSleepySatellite event in Salt Lake City on March 4, 2023. This was the first in a series of one-day hybrid conferences being held throughout the U.S. #BeyondSleepySatellite: Together in Salt Lake City... read >

On March 17, 2023, the Hypersomnia Foundation launches the premiere episode of LIVING WITH... a monthly YouTube series that expands awareness of idiopathic hypersomnia, healthy sleep habits, emerging research in sleep medicine, and more. Hosted by... read >

HAPPY 2023! If you’ve missed any of the latest news we’ve shared through our social media this month, don’t worry! Get up to date with the January edition of “In Case You Missed It!” Thank you for helping us reach our 2022 end-of-year... read >

Mark Your Calendar and Save the Dates! The Hypersomnia Foundation is planning multiple opportunities for all of us to get together in 2023! Plan on connecting with others in the sleep disorder community with these HF events: UNIGHT - Enjoy a virtual... read >
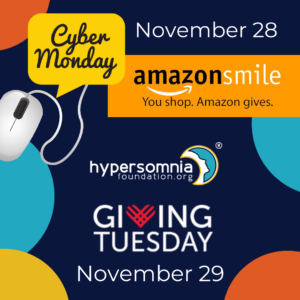
If you’ve missed any of the latest news we’ve shared through our social media this month, don’t worry! Get up to date with this edition of “In Case You Missed It!” Two ways you can support the Hypersomnia Foundation this holiday season... read >
November 29th is Giving Tuesday and we have much to be thankful for. We continue to listen to the community on our journey to improve as an organization for today and into the future. In June 2022, we hosted a successful #BeyondSleepy Conference for... read >
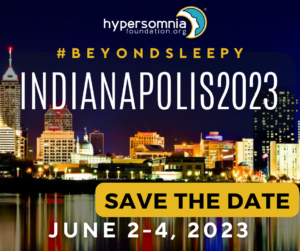
If you’ve missed any of the latest news we’ve shared through our social media this month, don’t worry! Get up to date with this edition of “In Case You Missed It!” Save the date for the HF 2023 #BeyondSleepy conference in Indianapolis!... read >

If you’ve missed any of the latest news we’ve shared through our social media this month, don’t worry! Get up to date with this edition of “In Case You Missed It!” Welcome Claire Crisp and Lindsay Jesteadt to the Hypersomnia Foundation... read >

If you’ve missed any of the latest news we’ve shared through our social media this month, don’t worry! Get up to date with this edition of “In Case You Missed It!” New medicine serdexmethylphenidate for IH set to enter clinical trials later... read >