SomnusNooze
 Since March 2015, over 2,300 people have joined the HF International Patient Registry at CoRDS. We now have a valuable dataset for researchers to study and a new research paper has just been published: “Disease Symptomatology and Response to Treatment in People with Idiopathic Hypersomnia: Initial Data from the Hypersomnia Foundation Registry”.* Our article summarizes the key findings of the research and what we have learned from it about idiopathic hypersomnia symptoms and treatments.
Since March 2015, over 2,300 people have joined the HF International Patient Registry at CoRDS. We now have a valuable dataset for researchers to study and a new research paper has just been published: “Disease Symptomatology and Response to Treatment in People with Idiopathic Hypersomnia: Initial Data from the Hypersomnia Foundation Registry”.* Our article summarizes the key findings of the research and what we have learned from it about idiopathic hypersomnia symptoms and treatments.
The research team was led by Dr. Lynn Marie Trotti, Chair of the Hypersomnia Foundation’s Medical Advisory Board. Rounding out the team are several faces familiar to the Hypersomnia Foundation community:
- Dr. Jason Ong, current Medical Advisory Board member
- Dr. David Plante, current Medical Advisory Board member
- Catherine Murray, former Hypersomnia Foundation Board member
- Rebecca King, current Hypersomnia Foundation Board member
- Dr. Donald Bliwise, sleep disorders researcher at Emory
The purpose of the analysis was to answer a few key questions about idiopathic hypersomnia (IH) symptoms and medication effectiveness. Let’s explore these questions one at a time.
What Symptoms Are Most Commonly Experienced Daily in IH?
Participants were asked about the frequency of symptoms experienced when they were “at their worst”. Nearly everyone with IH (97.7%) experienced excessive daytime sleepiness (EDS) every day. Brain fog and sleep inertia were the next most commonly experienced daily symptoms. The following chart shows the frequency of these and the other daily symptoms most commonly reported by people with IH.
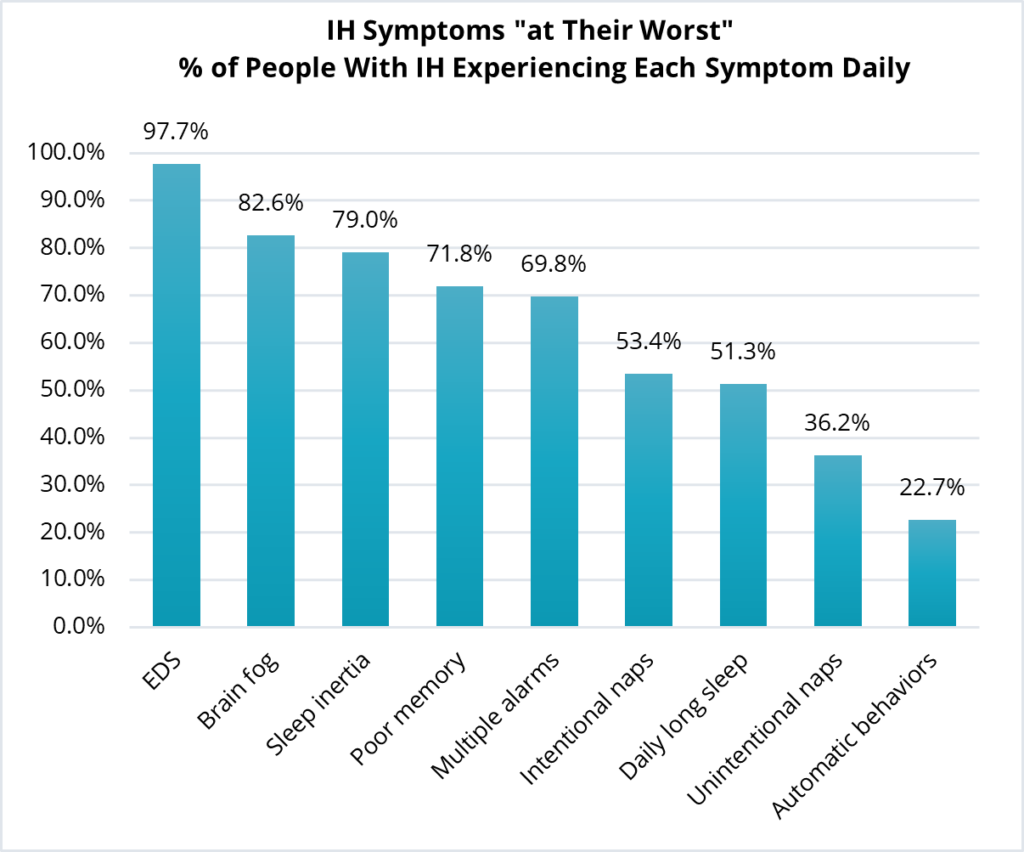
While EDS and difficulty awakening are symptoms used in the diagnosis of IH, cognitive symptoms such as brain fog and memory problems are not currently used for diagnosis. Although these symptoms are important to patients, they are difficult to measure and not well understood. More research is needed to understand these symptoms and how they affect an individual’s ability to be successful at work and school.
How Do the Above Most Commonly Experienced Daily Symptoms of IH Compare to the Symptoms Experienced Daily by People With Narcolepsy Types 1 and 2?
The frequency of symptoms experienced by people with IH “at their worst” did not differ markedly from the frequency experienced by those with narcolepsy types 1 or 2. Excessive daytime sleepiness (EDS) was stated by virtually everyone. Similar rates of daily long sleep durations, difficulty waking in the morning, need for multiple alarms, and cognitive symptoms occurred regardless of diagnosis. The only differences when symptoms were “at their worst” were that people with narcolepsy type 2 took more intentional naps than those with IH, and people with narcolepsy type 1 had more automatic behaviors and higher frequency of both intentional and unintentional naps.
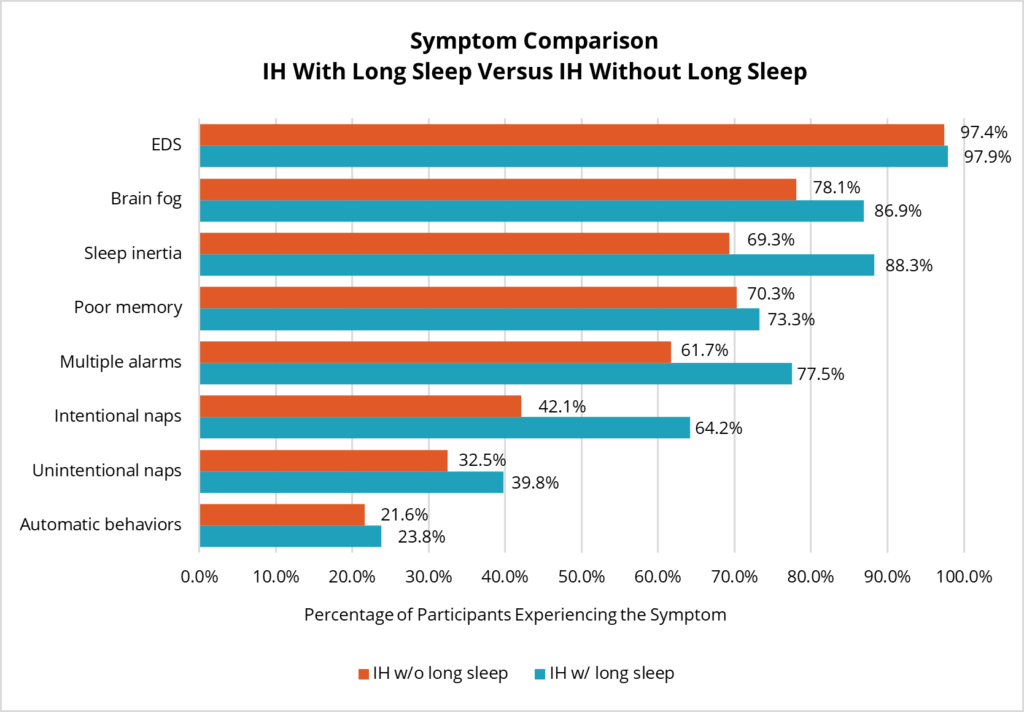
Do People With IH With Long Sleep Durations Have Different Symptoms Than Those Without Long Sleep Durations?
Researchers have noted that there may be two different phenotypes of IH demarcated by the length of uninterrupted nighttime sleep. Some people with IH have long, uninterrupted bouts of nighttime sleep (10 hours or longer) while others report getting a more typical 7-9 hours per night. A comparison of symptoms experienced daily by these two groups shows that those with long nighttime sleep duration are more likely to have trouble waking up and use multiple alarms. In addition, long nighttime sleep duration is associated with more frequent brain fog and the need to take intentional naps during the day. Nap duration was significantly longer in the long sleep time group. There was no significant difference in frequency of the other symptoms of IH.
What Medications Are Used Most Often to Treat IH, and How Well Do They Ease Symptoms?
An important finding regarding medication use in this registry was the relatively high proportion of IH respondents who were currently untreated with any medication for IH, nearly one in five. Most had tried at least one treatment and many had unsuccessfully tried several treatments.
For those being treated, the most commonly used treatments were amphetamine-dextroamphetamine (mixed amphetamine salts, 32%), followed by modafinil (30%) and methylphenidate (22%). Respondents with IH frequently reported previously taking these medications but discontinuing them—notably, 41% of participants with modafinil and 33% of participants with armodafinil. The survey did not ask why a respondent was not taking any medications or had discontinued a medication.
As participants were not only asked about their symptoms “at their worst” but also during the “last 30 days”, the research team compared symptoms between these two time periods for those with IH who were currently taking medications. All symptoms were at least somewhat improved, although we cannot know whether this is due to medication effectiveness or to fluctuations in symptoms unrelated to medications.
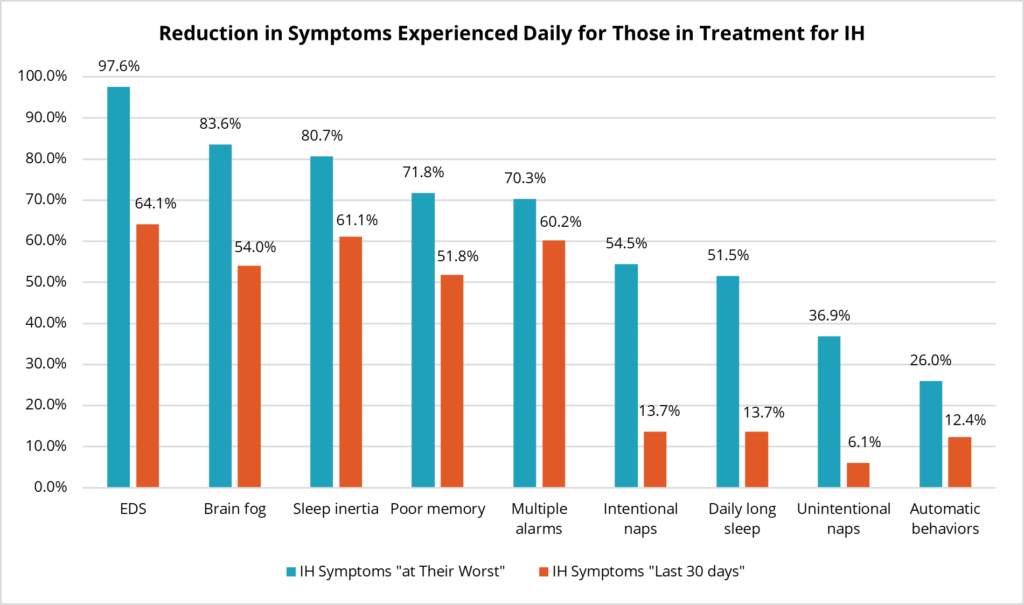
The high percentage of people with IH not taking any medications, the high discontinuation rate and the high amount of residual symptoms for people taking medications all speak to the ongoing, unmet clinical need for effective, tolerable treatments for IH.
Although the registry data does not tell us why people with IH stop taking medications, never try a specific medication, or take no medications at all, factors that may be contributing to medication decisions include:
- Failure of medications to relieve symptoms
- Side effects or considerations of other health conditions/medications
- Medications working for only a period of time, then no longer working
- High cost—insurance access and affordability issues
- Healthcare provider knowledge/awareness of treatment options
- Healthcare provider reluctance to prescribe certain medications
In summary, there is a great need for more effective medications, healthcare provider awareness and willingness to prescribe all IH treatments, and removal of institutional and cost barriers.
Final Thoughts
This paper would not have been possible without the participation of everyone who contributed their data to HF’s International Patient Registry at CoRDS. While the majority of current participants are non-Hispanic White females with IH from the U.S., we would like to encourage more individuals with other diagnoses and diverse backgrounds to join the registry. Not only will more diversity in the registry greatly improve the insights we may gain from future research, but the registry is an important tool for recruiting for clinical trials. While we welcome everyone to the registry, if you are male, LGBTQ+, live somewhere other than the U.S., or belong to a racial/ethnic group other than non-Hispanic White, your diversity has great value. The information you provide will be de-identified and kept strictly confidential. For more information (including a video of Dr. Trotti titled “HF’s Patient Registry at CoRDS”) and links to the registry, click here.
In the future, researchers would like to study how IH and related sleep disorders progress over time. If you are a registry participant and it’s been a year or more since your last annual update, please log in today and help us get the data we need for the next research study!
Thank you to everyone who participated in the registry, Dr. Lynn Marie Trotti, and the research team for your hard work and dedication to improving the lives of people with IH and related sleep disorders!
* Trotti, Lynn Marie, et al. “Disease Symptomatology and Response to Treatment in People with Idiopathic Hypersomnia: Initial Data from the Hypersomnia Foundation Registry.” Sleep Medicine, 2020, doi:10.1016/j.sleep.2020.08.034.
