SomnusNooze
 A recurring theme we see from people with idiopathic hypersomnia is an interest in finding others who share symptoms beyond sleepiness. This helps connect patients with common experiences and researchers on the path to finding causes and new and improved treatments.
A recurring theme we see from people with idiopathic hypersomnia is an interest in finding others who share symptoms beyond sleepiness. This helps connect patients with common experiences and researchers on the path to finding causes and new and improved treatments.
In the Spring of 2018, HF (via its social media, SomnusNooze, and its unique registry at CoRDS) helped researchers recruit people with IH and their supporters (to act as controls) for a study of autonomic dysfunction in IH. Autonomic dysfunction occurs when the autonomic nervous system (ANS) does not work properly. The ANS controls several basic functions, including blood pressure, heart rate, body temperature, breathing rate, digestion, skin sensation, bladder, and sweat function.
In May 2019, the researchers published an abstract as part of the annual meeting of the AAN (American Academy of Neurology). And now, the researchers have published an article entitled “Frequency and severity of autonomic symptoms in idiopathic hypersomnia” in the Journal of Clinical Sleep Medicine. Results showed that autonomic dysfunction is commonly associated with idiopathic hypersomnia. One of the study authors, Dr. Mitchell Miglis, has graciously provided the following summary of the journal article, along with a brief update about the future directions of this research.
Many patients with idiopathic hypersomnia (IH) report symptoms of autonomic impairment, such as lightheadedness on standing; fainting; problems with temperature regulation; and gastrointestinal dysfunction. However, studies on this topic are limited. We aimed to quantify the symptoms of autonomic nervous system dysfunction in a large online group of patients with IH, and to determine how these symptoms interact with sleepiness, fatigue, and quality of life.
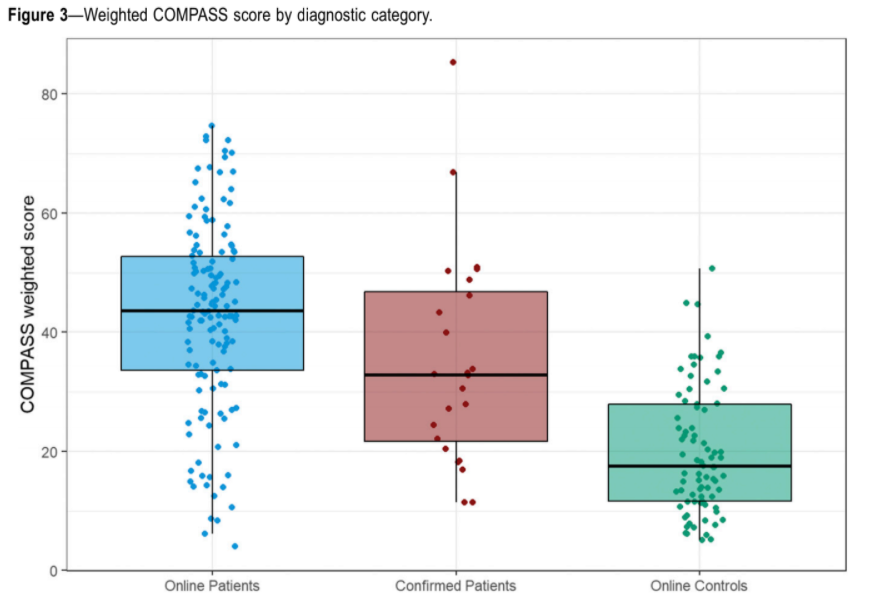
One hundred thirty-eight patients with IH and 81 age- and sex-matched controls were recruited via the Hypersomnia Foundation. To validate our findings, we selected 24 of our own confirmed IH patients and had them complete the same surveys. All participants completed a battery of online sleep, autonomic, and quality of life questionnaires, including the composite autonomic symptom score-31 (COMPASS-31), a standardized survey of autonomic function with several subdomains including gastrointestinal, genitourinary, etc.
We found that both groups of people with IH, the online-recruited and the physician-confirmed, reported significantly higher COMPASS-31 autonomic scores, with the greatest symptom burden in the orthostatic (lightheadedness) and vasomotor (peripheral blood vessel regulation) domains (see figure).
Online and confirmed patients reported more sleepiness, whereas only online patients reported more fatigue. Both sleepiness and fatigue were positively correlated with COMPASS-31 autonomic scores. In other words, patients with more autonomic dysfunction (measured via COMPASS-31 scores) reported more sleepiness and fatigue.
Patients reported lower quality of life, as reflected by lower scores across all domains of the RAND 36-item health survey, which was negatively correlated with COMPASS-31 scores. In other words, the worse the patient’s autonomic function (higher COMPASS-31 score), the more severe their sleepiness and fatigue, and the worse their quality of life was (lower RAND-36 score).
Many patients reported other diagnoses of autonomic dysfunction, with the most common being postural tachycardia syndrome (POTS). We also found that many reported allergic symptoms concerning for mast cell activation syndrome (MCAS), which frequently co-exists with POTS.
Future Directions:
We are continuing our research in this arena and are currently in the process of analyzing objective measures of autonomic function testing in patients with IH. An important goal is to probe deeper into the underlying mechanism of this interesting correlation, which may help determine underlying causes and/or better treatments for IH and for autonomic disorders.
Note: For more information on POTS and its relationship with idiopathic hypersomnia, see this Ask the Doctor article.
