SomnusNooze e-newsletter
News, stories and updates from the world of sleep
News, stories and updates from the world of sleep
A Pilot Study of tDCS Looks Promising for the Treatment of Idiopathic Hypersomnia Background Idiopathic hypersomnia (IH) can severely impact affected individuals’ family, employment, education, and leisure activities. And because there are no... read >
Question: Is there an overlap between idiopathic hypersomnia and type 2 narcolepsy? Answer: The short answer to this question is yes. The only way to definitively distinguish idiopathic hypersomnia (IH) from type 2 narcolepsy (T2N) is the number of... read >

Social Security Disability Series: Part 2 By Anjel Burgess, JD For Part 1 in this series, click HERE. For Ms. Burgess' presentation at our 2018 conference, click HERE. Jennie has been fortunate enough to secure her short-term disability benefits. She... read >
Very recently, the Hypersomnia Foundation became aware of an opportunity to help shape the future of sleep research. The National Institutes of Health, the primary source of funding for medical research in the United States, has issued a Request... read >
If you haven’t made your plans yet to attend the Hypersomnia Foundation’s regional conference in Denver—Beyond Sleepy in the Mile High City—you might want to do so today. Tickets are selling fast and seating is limited. The big event is in less... read >
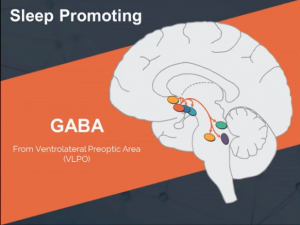
A study of clarithromycin in the treatment of GABA-related hypersomnia indicates that this drug may be effective in some patients with idiopathic hypersomnia (IH), narcolepsy without cataplexy, and subjective hypersomnia. Background The US Food and... read >
The Hypersomnia Foundation has become aware that Pavilion Pharmacy, a provider of flumazenil cream and sublingual lozenges in the United States, has been unable to fill new or renewing prescriptions for this drug. We have contacted the company owner and... read >

I guess my story is a lot like other people’s stories. . .or at least I hope it's a lot like theirs. My symptoms started when I was about 14 years old. Actually, except for my early childhood, I don't really remember being awake a lot. In school, I... read >
An article published on May 11, 2015, in U.S. News & World Report highlights the struggles of two women whose lives are challenged by idiopathic hypersomnia. They are, as reporter Anna Miller explains, “at the sandman's beck and call.” One... read >
Did you miss this event? Click to watch the recording! Click the calendar link for more info. The Hypersomnia Foundation presents Snooze TV Episode 2 which includes a guest panel of... read >