SomnusNooze e-newsletter
News, stories and updates from the world of sleep
News, stories and updates from the world of sleep
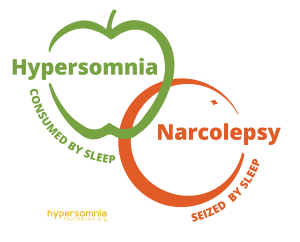
Question: Is there an overlap between idiopathic hypersomnia and type 2 narcolepsy? Answer: The short answer to this question is yes. The only way to definitively distinguish idiopathic hypersomnia (IH) from type 2 narcolepsy (T2N) is the number of... read >