SomnusNooze e-newsletter
News, stories and updates from the world of sleep
News, stories and updates from the world of sleep
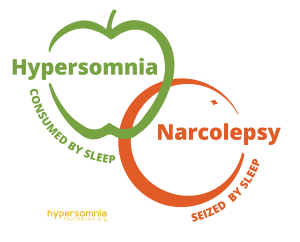
Question: Is there an overlap between idiopathic hypersomnia and type 2 narcolepsy? Answer: The short answer to this question is yes. The only way to definitively distinguish idiopathic hypersomnia (IH) from type 2 narcolepsy (T2N) is the number of... read >

Social Security Disability Series: Part 2 By Anjel Burgess, JD For Part 1 in this series, click HERE. For Ms. Burgess' presentation at our 2018 conference, click HERE. Jennie has been fortunate enough to secure her short-term disability benefits. She... read >
Very recently, the Hypersomnia Foundation became aware of an opportunity to help shape the future of sleep research. The National Institutes of Health, the primary source of funding for medical research in the United States, has issued a Request... read >
If you haven’t made your plans yet to attend the Hypersomnia Foundation’s regional conference in Denver—Beyond Sleepy in the Mile High City—you might want to do so today. Tickets are selling fast and seating is limited. The big event is in less... read >

Background Compared with adults with narcolepsy, children with narcolepsy often have higher levels of excessive daytime sleepiness (EDS), are more likely to have cataplexy without a trigger, and are more likely to have a secondary form of narcolepsy. The... read >
Did you miss this event? Click to watch the recording! Click the calendar link for more info. The Hypersomnia Foundation presents Snooze TV Episode 3 which includes a guest panel of narcolepsy... read >
On September 24, 2013, the US Food and Drug Administration (FDA) held a public meeting to solicit information on the impact of narcolepsy on affected individuals’ daily lives and the effect of currently available medication on their disease symptoms. A... read >
A symposium entitled, “Idiopathic Hypersomnia: Past, Present and Future,” and co-chaired by Drs. Michel Billiard (Montpellier, France) and Sona Nevsimalova (Charles University, Prague, Czech Republic), took place at the World Association of Sleep... read >