SomnusNooze e-newsletter
News, stories and updates from the world of sleep
News, stories and updates from the world of sleep
Question: Is there an overlap between idiopathic hypersomnia and type 2 narcolepsy? Answer: The short answer to this question is yes. The only way to definitively distinguish idiopathic hypersomnia (IH) from type 2 narcolepsy (T2N) is the number of... read >

Social Security Disability Series: Part 2 By Anjel Burgess, JD For Part 1 in this series, click HERE. For Ms. Burgess' presentation at our 2018 conference, click HERE. Jennie has been fortunate enough to secure her short-term disability benefits. She... read >
If you haven’t made your plans yet to attend the Hypersomnia Foundation’s regional conference in Denver—Beyond Sleepy in the Mile High City—you might want to do so today. Tickets are selling fast and seating is limited. The big event is in less... read >
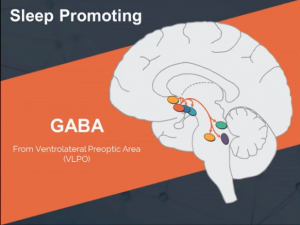
A study of clarithromycin in the treatment of GABA-related hypersomnia indicates that this drug may be effective in some patients with idiopathic hypersomnia (IH), narcolepsy without cataplexy, and subjective hypersomnia. Background The US Food and... read >
Dr. David Rye's 2013 session at the Narcolepsy Network conference entitled: What's in a Name? Understanding the Origins of the Terminologies for the Family of Hypersomnias. A fascinating examination of semantics and the signs and symptoms of... read >
On September 24, 2013, the US Food and Drug Administration (FDA) held a public meeting to solicit information on the impact of narcolepsy on affected individuals’ daily lives and the effect of currently available medication on their disease symptoms. A... read >