SomnusNooze e-newsletter
News, stories and updates from the world of sleep
News, stories and updates from the world of sleep

HAPPY 2023! If you’ve missed any of the latest news we’ve shared through our social media this month, don’t worry! Get up to date with the January edition of “In Case You Missed It!” Thank you for helping us reach our 2022 end-of-year... read >
Why do Emory University’s sleep researchers perform spinal tap procedures on sleepy patients? What is the “sleepy juice” they’re looking for in the spinal fluid? Does it have anything to do with prostaglandins? An expert answers all these... read >

MAY 2021 IMPORTANT ADDENDUM: This article and its associated video presentation is now outdated. In May 2021, Hypersomnia Foundation released updated content based on this presentation. Please see the following links for updated information:... read >

Do children with ADHD have a higher risk for narcolepsy? Could complex sleep apnea be related to problems with the vagus nerve? A medical expert answers! We are delighted to have Dr. Kiran Maski of Harvard Medical School, a renowned expert in pediatric... read >
Happy March! Did you know that March is Women’s History Month? While you are celebrating all the amazing women throughout history this entire month, don’t forget that there are also lots of other fun (and offbeat) celebrations in March, including... read >
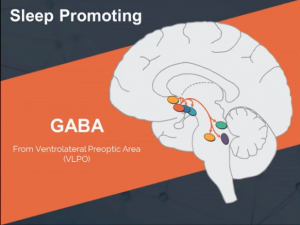
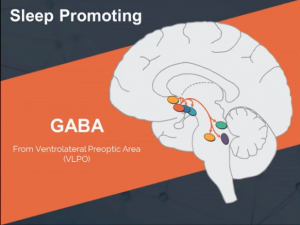
What is GABA? What role does it play in sleep? And is GABA activity increased by something in the cerebrospinal fluid of people with hypersomnia? We are very pleased to present Part 2 of a new two-part series by neuroscientist Amanda Freeman, PhD, of... read >

Happy February! This month is full of celebrations – the Lunar New Year (it’s the Year of the Pig), Black History Month, Presidents’ Day, and the sweetest day of all – Valentine’s Day! But since February is also the shortest month, that means... read >
In December’s SomnusNooze, we featured Part 1 of a 2-part Summary of the research findings presented at the 7th International Symposium on Narcolepsy, which was held earlier this fall in Boston. Prominent sleep medicine researchers and physicians,... read >
What is GABAA? And how does it affect hypersomnia? We are very pleased to present a two-part video series by neuroscientist Amanda Freeman, PhD, of Emory University, which describes, in layman’s terms, exactly how y-aminobutyric acid, better known as... read >
Happy 2019! As we welcome the new year, we at the Hypersomnia Foundation have resolved to make things easier for our followers! In this month’s “In Case You Missed It!,” we highlight some of the most important news and social media posts about the... read >